Ihre Nachricht wurde gesendet.
Wir werden Ihre Anfrage bearbeiten und uns so schnell wie möglich mit Ihnen in Verbindung setzen.
Das Formular wurde erfolgreich abgeschickt.
Weitere Informationen finden Sie in Ihrem Briefkasten.

Sprache auswählen


Der Bedarf der Menschen an psychosozialer Unterstützung wächst schneller, als das Gesundheitssystem es bewältigen kann. In den USA, 1 von 5 Personen bei denen eine psychische Störung diagnostiziert wurde, und rund 17% der Bevölkerung mit Drogenmissbrauch zu tun hat. All diese Menschen benötigen qualifizierte psychosoziale Dienste.
Aber bekommen sie sie auch? Nun, nein. Auch wenn 70% der Amerikaner leben in Gebieten, die von Organisationen für psychische Gesundheit abgedeckt werden, nur etwa 27,7% der Menschen tatsächlich Hilfe bekommen.
Aus diesem Grund ist die Entwicklung von Apps für die psychische Gesundheit ein heißes Thema in 2026. Und wie so oft sehe ich Leute, die sich in die Entwicklung stürzen, ohne genau zu wissen, was sie (und ihre Nutzer) brauchen. Sie rennen den neuesten Modetrends hinterher und stecken dann mit Apps fest, die heruntergeladen werden und kurz darauf in Vergessenheit geraten.
In diesem Artikel werde ich aufschlüsseln, wie man eine App für psychische Gesundheit in 2026 die richtige Art und Weise: die wichtigen Funktionen, die zu vermeidenden Fallstricke und einige Lektionen, die mein Team bei Innowise und ich gelernt haben.
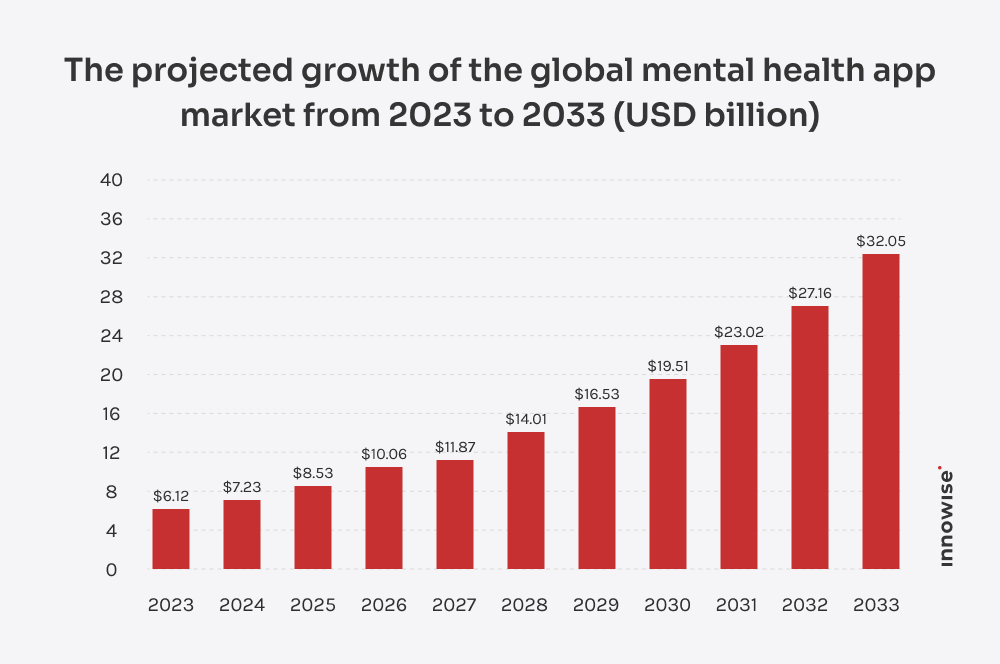
Apps für die psychische Gesundheit werden zu einem wichtigen Bestandteil der Art und Weise, wie Menschen ihr Wohlbefinden steuern. Lassen Sie uns die Zahlen durchgehen. Im Jahr 2024 war der globale Markt für die Entwicklung von Apps für die psychische Gesundheit bereits im Wert von $7,23 Milliarden, und es wird erwartet, dass es die $32.05 Milliarden bis 2034 mit einem 18% CAGR.
Was ist der Grund für diesen Anstieg? Zum Teil ist es kulturell bedingt. Das Stigma, über Depressionen, Angstzustände oder Sucht zu sprechen, schwindet, insbesondere bei jüngeren Menschen. Über 38% der Amerikaner nutzen bereits die Telemedizin, um Fachleute für psychische Gesundheit aufzusuchen, und fast 59% sagen, sie seien offen für diese Möglichkeit. Gleichzeitig ist der Zugang zu herkömmlichen Therapien nach wie vor begrenzt, so dass Apps für die psychische Gesundheit genau ins Schwarze treffen.
Außerdem sind Apps für die psychische Gesundheit dank des technischen Fortschritts viel praktischer als die Tools von vor ein paar Jahren. Mein Team und ich haben diesen Wandel aus erster Hand erlebt: Anbieter und Startup-Gründer kommen nicht mehr zu Anbieter von Lösungen für das Gesundheitswesen IT wie Innowise, die nach einem einfachen Stimmungsaufzeichnungsgerät fragen. Sie wollen neue Funktionen, die ihren Nutzern einen Mehrwert bieten, wie AI-basierte Chat-Unterstützung, personalisierte CBT-Module und integrierte Wearables.
Sicher, die Entwicklung von Apps für die psychische Gesundheit bringt eine Reihe von Herausforderungen mit sich: komplexe Compliance-Anforderungen, die Sorge der Nutzer um ihre sensiblen Daten und der starke Wettbewerb auf dem Markt. Aber ich greife mir selbst vor - lassen Sie uns zuerst über die guten Dinge sprechen.
Nur Apps für die psychische Gesundheit, die echte Ergebnisse bringen, halten dem Test der Zeit stand. Hier sind einige Vorteile, die ich am häufigsten in erfolgreichen Fällen sehe.
In vielen Teilen der USA beträgt die durchschnittliche Wartezeit auf einen Termin bei einem Psychiater 67 Tage. Stellen Sie sich vor: Das sind über zwei Monate, in denen Sie sich ohne professionelle Unterstützung abmühen. Mit Telemedizin, die durchschnittliche Wartezeit sinkt auf 43 Tage. Es ist kein sofortiger Zugang, aber es kann einen Unterschied machen. In der Zwischenzeit bieten die Apps klinisch erprobte Stressbewältigungsmechanismen und das Gefühl von Gemeinschaft.
Für viele Menschen kann der Gang zu einem Therapeuten überwältigend sein, vor allem wenn die Scham, gesehen zu werden, im Weg steht. Apps beseitigen diese Barrieren, denn sie ermöglichen es den Menschen, privat Hilfe zu suchen und früher mit der psychologischen Betreuung zu beginnen.
In Krisenmomenten können Funktionen wie Chatbots oder angeleitete Übungen die Lücke füllen, bis professionelle Unterstützung verfügbar ist. Apps für psychische Gesundheit ermöglichen es den Menschen, Symptome zu verfolgen, Stimmungen zu protokollieren und Auslöser in Echtzeit zu managen. Die Forschung zeigt, dass insbesondere Chatbots großes Potenzial für die Bereitstellung sozialer und psychologischer Unterstützung wenn menschliche Interaktion nicht unmittelbar möglich ist.
Leider ist das Hindernis für eine Therapie oft der Preis, und Apps für psychische Gesundheit machen die Behandlung erschwinglicher. Für eine relativ niedrige Abonnementgebühr erhalten die Menschen geführte Programme, Unterstützung durch die Gemeinschaft und strukturierte Übungen, die sie offline nicht bekommen könnten.
Für Kliniken und einzelne Therapeuten eröffnen die Apps neue Geschäftsmöglichkeiten. Anstatt auf ein Büro oder eine lokale Region beschränkt zu sein, können Anbieter ihre Dienstleistungen geografisch ausweiten.
Wenn Sie mit der Entwicklung einer App für psychische Gesundheit beginnen, sollten Sie sich frühzeitig entscheiden, welche Art von App Sie entwickeln wollen. Jede spielt eine andere Rolle bei der psychischen Gesundheit: Einige bieten den Nutzern schnelle Stressentlastung, andere strukturierte Therapiesitzungen. Obwohl sich die Kategorien oft überschneiden, lassen sich die meisten Apps in einige wenige Typen einteilen.
Diese Apps helfen den Nutzern, tägliche Gewohnheiten in Bezug auf Achtsamkeit, Entspannung, emotionale Belastbarkeit und geistiges Wohlbefinden zu entwickeln. Ein gutes Beispiel ist die Mobile Meditationssuite die unser Team entwickelt hat. Sie Steigerung der Nutzerbindung und des Engagements um 41% durch die Kombination von immersiver VR mit traditionellen Meditationswerkzeugen.
Mit diesen Apps können Menschen ihre Emotionen aufzeichnen, Symptome notieren und Aktivitäten wie Schlaf, Bewegung und Medikamente verfolgen. Mit der Zeit wird aus den Daten eine persönliche Aufzeichnung, die Muster und Auslöser aufzeigen kann. Mein Team arbeitete an einer AI-gespeiste Depressionserkennung Plattform, die EEG-Eingaben analysierte, um Frühwarnzeichen der Krankheit zu erkennen.
Diese reichen von Symptom-Checkern für psychische Störungen bis hin zu Tools für therapeutische Interventionen und Notfallhilfe. Im Gegensatz zu allgemeinen Wellness-Apps müssen SaMD strenge Zulassungsprozesse (FDA, MDR) durchlaufen und werden häufig klinischen Studien unterzogen. Neben Programmierkenntnissen erfordert die Entwicklung in diesem Bereich tiefgreifende Kenntnisse der Compliance- und Validierungsprozesse.
Erleben Sie, wie unsere Entwickler von Apps für psychische Gesundheit Ihre Idee in ein vollwertiges Produkt umsetzen.
Die Funktionen von Apps für psychische Gesundheit können je nach Zweck und Zielgruppe sehr unterschiedlich sein. Allerdings gibt es bestimmte Funktionen in vielen Apps für psychische Gesundheit, unabhängig von ihrem Schwerpunkt. Im Folgenden haben wir einige der gängigsten Funktionen aufgeführt.
Tagebucheinträge, Stimmungsprotokolle und die Verfolgung des Lebensstils vermitteln den Nutzern ein klares Bild davon, wie es ihnen Tag für Tag geht. Gepaart mit geführten Meditationen, Achtsamkeitsübungen, beruhigenden Videos oder CBT-basierten Übungen helfen diese Funktionen den Menschen, Schritte zu einem besseren Wohlbefinden zu unternehmen.

Die integrierte Telemedizin ermöglicht es, Online-Konsultationen zu vereinbaren, privat mit Anbietern zu chatten, an Videokonsultationen teilzunehmen und eine diensthabende Fachkraft anzurufen, wenn dringend Hilfe benötigt wird. Für Menschen, die weit entfernt von psychiatrischen Kliniken leben, wird die App so zu einem Rettungsanker.

Apps für psychische Gesundheit enthalten spielähnliche Elemente wie Belohnungen und Herausforderungen. Die Nutzer können Punkte und Abzeichen verdienen oder Aktivitätsserien wie Atemübungen oder Meditationen absolvieren. Es mag unbedeutend klingen, aber solche Funktionen motivieren die Menschen, mit der Behandlung fortzufahren.

Apps, die Inhalte an verschiedene Altersgruppen, kulturelle Kontexte oder persönliche Ziele anpassen, wirken relevanter und binden die Nutzer länger. Personalisierung bedeutet oft, dass mehrere Designmodi angeboten werden oder Routinen auf der Grundlage früherer Aktivitäten vorgeschlagen werden.

Fortschrittsanzeigen verwandeln kleine Erfolge in sichtbare Impulse: ein beständigerer Schlafrhythmus, weniger Panikattacken oder einfach nur das tägliche Führen eines Tagebuchs. Zielsetzungsfunktionen gehen noch einen Schritt weiter, indem sie den Nutzern spezifische Meilensteine vorgeben, die sie ansteuern können.

Die Krisenmanagement-Funktionen von Apps für psychische Gesundheit bieten sofortige Unterstützung bei akuten Notlagen. Dazu gehören Panik-Buttons, die den Standort des Nutzers mit einer vertrauenswürdigen Kontaktperson teilen, sofortige Anrufe bei Krisenhotlines oder Video-Notrufleitungen mit Fachleuten.

Gemeinschaftsbereiche, wie moderierte Foren, Gruppenchats oder Live-Gruppenmeditationssitzungen, helfen den Nutzern, Erfahrungen auszutauschen und sich gegenseitig zu ermutigen. In Kombination mit professioneller Anleitung können Community-Funktionen das Gefühl vermitteln, dass die Menschen mit ihren Problemen nicht allein sind.

Unternehmen können den Nutzern die erbrachten Dienste sofort in Rechnung stellen, beispielsweise durch Zahlungen pro Sitzung oder ein App-Abonnement. Wenn die Versicherung die Dienste nicht abdeckt, können die Nutzer über integrierte Zahlungsgateways mit ihren Debitkarten, Kreditkarten oder mobilen Geldbörsen bezahlen.

Mit einer Terminplanungsfunktion können Nutzer Offline-Sitzungen mit Therapeuten direkt in der App buchen. In Verbindung mit der Kalenderintegration werden so verpasste Termine reduziert und die Therapie bleibt strukturiert. Für den Anbieter bedeutet das auch weniger Verwaltungsaufwand und weniger Nicht-Erscheinen.

Push-Benachrichtigungen und Erinnerungen sorgen dafür, dass die Nutzer ihre Therapiepläne einhalten. Zum Beispiel, indem man jemanden anregt, ein tägliches Stimmungsprotokoll zu führen, ihn an einen bevorstehenden Termin erinnert oder eine Meditation nach einem stressigen Tag vorschlägt.

Tagebucheinträge, Stimmungsprotokolle und die Verfolgung des Lebensstils vermitteln den Nutzern ein klares Bild davon, wie es ihnen Tag für Tag geht. Gepaart mit geführten Meditationen, Achtsamkeitsübungen, beruhigenden Videos oder CBT-basierten Übungen helfen diese Funktionen den Menschen, Schritte zu einem besseren Wohlbefinden zu unternehmen.

Die integrierte Telemedizin ermöglicht es, Online-Konsultationen zu vereinbaren, privat mit Anbietern zu chatten, an Videokonsultationen teilzunehmen und eine diensthabende Fachkraft anzurufen, wenn dringend Hilfe benötigt wird. Für Menschen, die weit entfernt von psychiatrischen Kliniken leben, wird die App so zu einem Rettungsanker.

Apps für psychische Gesundheit enthalten spielähnliche Elemente wie Belohnungen und Herausforderungen. Die Nutzer können Punkte und Abzeichen verdienen oder Aktivitätsserien wie Atemübungen oder Meditationen absolvieren. Es mag unbedeutend klingen, aber solche Funktionen motivieren die Menschen, mit der Behandlung fortzufahren.

Apps, die Inhalte an verschiedene Altersgruppen, kulturelle Kontexte oder persönliche Ziele anpassen, wirken relevanter und binden die Nutzer länger. Personalisierung bedeutet oft, dass mehrere Designmodi angeboten werden oder Routinen auf der Grundlage früherer Aktivitäten vorgeschlagen werden.

Fortschrittsanzeigen verwandeln kleine Erfolge in sichtbare Impulse: ein beständigerer Schlafrhythmus, weniger Panikattacken oder einfach nur das tägliche Führen eines Tagebuchs. Zielsetzungsfunktionen gehen noch einen Schritt weiter, indem sie den Nutzern spezifische Meilensteine vorgeben, die sie ansteuern können.

Die Krisenmanagement-Funktionen von Apps für psychische Gesundheit bieten sofortige Unterstützung bei akuten Notlagen. Dazu gehören Panik-Buttons, die den Standort des Nutzers mit einer vertrauenswürdigen Kontaktperson teilen, sofortige Anrufe bei Krisenhotlines oder Video-Notrufleitungen mit Fachleuten.

Gemeinschaftsbereiche, wie moderierte Foren, Gruppenchats oder Live-Gruppenmeditationssitzungen, helfen den Nutzern, Erfahrungen auszutauschen und sich gegenseitig zu ermutigen. In Kombination mit professioneller Anleitung können Community-Funktionen das Gefühl vermitteln, dass die Menschen mit ihren Problemen nicht allein sind.

Unternehmen können den Nutzern die erbrachten Dienste sofort in Rechnung stellen, beispielsweise durch Zahlungen pro Sitzung oder ein App-Abonnement. Wenn die Versicherung die Dienste nicht abdeckt, können die Nutzer über integrierte Zahlungsgateways mit ihren Debitkarten, Kreditkarten oder mobilen Geldbörsen bezahlen.

Mit einer Terminplanungsfunktion können Nutzer Offline-Sitzungen mit Therapeuten direkt in der App buchen. In Verbindung mit der Kalenderintegration werden so verpasste Termine reduziert und die Therapie bleibt strukturiert. Für den Anbieter bedeutet das auch weniger Verwaltungsaufwand und weniger Nicht-Erscheinen.

Push-Benachrichtigungen und Erinnerungen sorgen dafür, dass die Nutzer ihre Therapiepläne einhalten. Zum Beispiel, indem man jemanden anregt, ein tägliches Stimmungsprotokoll zu führen, ihn an einen bevorstehenden Termin erinnert oder eine Meditation nach einem stressigen Tag vorschlägt.

Künstliche Intelligenz ist kein Wundermittel für die psychische Gesundheit, aber wenn es mit Bedacht eingesetzt wird, kann es Apps viel nützlicher und persönlicher machen. Der Schlüssel liegt in der Auswahl von Funktionen, die tatsächlich einen Mehrwert bieten. Hier sind einige, die in Projekten, an denen mein Team und ich gearbeitet haben, immer wieder einen Unterschied gemacht haben.
Wenn man mit der Entwicklung einer App für psychische Gesundheit beginnt (wie bei jeder anderen App auch), sind Herausforderungen unvermeidlich. Der Schlüssel ist, nicht von ihnen überrumpelt zu werden. Hier sind einige der Herausforderungen, die ich in diesem Bereich häufig sehe, und Bewältigungsstrategien, die wirklich funktionieren.
Das Wesentliche: Die Nutzer müssen davon überzeugt sein, dass die App für psychische Gesundheit tatsächlich funktioniert und sinnvolle Ergebnisse liefert, sonst werden sie sie schnell wieder aufgeben.
Wie man sie überwindet: Die Nutzer sollten schnell einen Nutzen erkennen. Das bedeutet, dass das Onboarding praktische Funktionen und Ergebnisse hervorheben sollte. Untermauern Sie Ihre Behauptungen mit Beweisen: Führen Sie klinische Forschungen an, heben Sie die Referenzen von Therapeuten hervor oder teilen Sie anonymisierte Erfolgsgeschichten, um zu beweisen, dass die App nicht nur ein weiteres Wellness-Gimmick ist. Außerdem würde ich den Schwerpunkt auf Konsistenz, zuverlässige App-Leistung und genaue Erkenntnisse legen.
Das Wesentliche: Apps für psychische Gesundheit verwenden geschützte Gesundheitsdaten, was die Einhaltung von HIPAA und GDPR voraussetzt, und überschneiden sich manchmal mit SaMD, was bedeutet, dass sie eine FDA- oder MDR-Genehmigung benötigen.
Wie man sie überwindet: Am klügsten ist es, die Einhaltung von Vorschriften bereits bei der Produktentwicklung zu berücksichtigen. Zeichnen Sie jeden Datenfluss frühzeitig auf und stellen Sie sicher, dass er mit den rechtlichen Rahmenbedingungen übereinstimmt. Wenn Sie eine App für psychische Gesundheit intern entwickeln, empfehle ich Ihnen, einen IT-Berater für das Gesundheitswesen zu engagieren, der sich mit den Compliance-Rahmenbedingungen auskennt, um das Projekt auf Kurs zu halten.
Das Wesentliche: Apps, die zu viel versprechen, sich auf ungeprüfte AI-Ergebnisse stützen oder Krisen falsch handhaben, können echten Schaden anrichten.
Wie man sie überwindet: Ziehen Sie eine klare Grenze zwischen dem, was die App kann und was sie nicht kann, und kommunizieren Sie dies den Nutzern aufrichtig. Wenn AI für Empfehlungen oder Stimmungserkennung verwendet wird, sollte es immer als Unterstützung und nicht als Ersatz für professionelle Pflege positioniert werden. Sie sollten klare Eskalationswege für Krisensituationen einrichten, wie z. B. Hotlines oder die Integration von Notdiensten.
Das Wesentliche: Der Markt für Apps zur psychischen Gesundheit ist ziemlich überfüllt, und viele Apps konkurrieren um Aufmerksamkeit.
Wie man sie überwindet: Anstatt die Funktionen zu kopieren, die alle anderen haben, sollten Sie sich auf einen bestimmten Schmerzpunkt der Nutzer konzentrieren und diesen besser lösen als alle anderen auf dem Markt für Apps zur psychischen Gesundheit. Die Positionierung in der Nische wird schneller an Zugkraft gewinnen. Ich empfehle außerdem, in Funktionen zur Kundenbindung zu investieren (Personalisierung, Gamification, kontinuierliche Feedbackschleifen), damit die Nutzer nicht abspringen.
Nachdem ich nun die wichtigsten Funktionen und Herausforderungen erläutert habe, kommen wir zum Wesentlichen: Wie kann man eine erfolgreiche App für psychische Gesundheit entwickeln? Auf diese Frage gibt es keine einfache Antwort. Aber oft läuft alles auf diese einfachen Wahrheiten hinaus.
Die Ende-zu-Ende-Verschlüsselung schützt die Daten, egal ob sie gespeichert oder gesendet werden, und die Multi-Faktor-Authentifizierung stellt sicher, dass nur die richtigen Personen Zugang erhalten. Darüber hinaus trägt die Integration dieser Maßnahmen zum Schutz von Daten im Einklang mit gesetzlichen Anforderungen wie HIPAA und GDPR bei.
Patienten und Therapeuten verwenden unterschiedliche Geräte, wie iOS- oder Android-Smartphones oder Computer mit macOS oder Windows. Aber sie erwarten, dass die App auf beiden Geräten auf die gleiche Weise funktioniert. Wenn das nicht der Fall ist (oder schlimmer noch - die App überhaupt nicht funktioniert), riskieren Sie, einen großen Teil der Zielgruppe zu verprellen.
Wearables, wie Smartwatches, Sensoren und Schlaftracker, verleihen Apps für die psychische Gesundheit eine neue Dimension. Die Einbeziehung der Herzfrequenzvariabilität oder von Schlafdaten kann beispielsweise die Sichtweise der Nutzer auf ihre Stressmuster verändern. Selbst etwas Einfaches, wie die Anregung zu einer Atemübung nach einem stressigen Tag, lässt die App persönlich und hilfreich erscheinen.
Wenn das Design einer App für psychische Gesundheit die Nutzer verwirrt oder überfordert, werden sie nicht wiederkommen, ganz gleich, wie fortschrittlich die Funktionen sind. Das Design muss einfach, beruhigend und zugänglich sein.
Der Versuch, die HIPAA- oder GDPR-Konformität am Ende aufzuschrauben, ist komplex und wird die Einführung definitiv verzögern. Jede Funktion, die mit Daten in Berührung kommt, wie Chat, Journaling oder Videositzungen, muss von Anfang an unter Berücksichtigung der Vorschriften entwickelt werden.
Die erfolgreichen Apps für die psychische Gesundheit wachsen fast immer zu schnell über ihr anfängliches Design hinaus. Ich habe erlebt, dass sich die erwartete Nutzerbasis einer App innerhalb weniger Monate verdoppelt oder verdreifacht hat, und plötzlich kann das System den Datenverkehr nicht mehr bewältigen. Die Planung für die Skalierung (mehr Nutzer, mehr Daten oder neue Integrationen) verhindert, dass Sie sich verzweifeln, wenn sich der Erfolg einstellt.
Die Entwicklung einer App für psychische Gesundheit kann sich beim ersten Mal überwältigend anfühlen. Es gibt unzählige bewegliche Teile - Auswahl von Funktionen, Einhaltung von Vorschriften, Zeitvorgaben - und man unterschätzt leicht die Risiken. Mein Rat: Versuchen Sie nicht, alles allein zu machen. Die Zusammenarbeit mit einem Team, das bereits Software für das Gesundheitswesen entwickelt hat, erspart Ihnen die klassischen Fehler und monatelange Nacharbeit.
Mein Team bei Innowise geht bei der Entwicklung von Apps für die psychische Gesundheit in der Regel folgendermaßen vor.
An dieser Stelle setzen wir uns mit den Beteiligten zusammen und gestalten das Konzept der App für psychische Gesundheit. Das Team von Innowise stellt Fragen, um die Zielgruppe, die optimale Funktionalität und die erwarteten geschäftlichen Auswirkungen zu verstehen.
Sobald die Vision festgelegt ist, definieren wir die funktionalen und nicht-funktionalen Anforderungen an die Software für psychische Gesundheit. Das heißt, wir dokumentieren Funktionen, Sicherheit, Datenschutz und Compliance.
Hier wählen wir den technischen Stack aus und entwerfen die Architektur. In dieser Phase planen wir auch die Umsetzung der gesetzlich vorgeschriebenen Sicherheits- und Datenschutzmaßnahmen.
Danach erstellen wir einen klaren Projektplan: Wir planen das Projektbudget, weisen die Ressourcen zu, legen den Zeitplan fest und definieren die wichtigsten Projektmeilensteine, wobei wir auch mögliche Risiken berücksichtigen.
In dieser Phase geht es nicht nur um die Optik, sondern auch um die Zugänglichkeit und die Emotionen der Nutzer. Unsere UX/UI-Designer erstellen Wireframes und Prototypen, die genau zeigen, wie die Nutzer mit der App interagieren werden.
Unsere Entwickler von Apps für psychische Gesundheit erstellen das Front-End und Back-End in 2-3-wöchigen Sprints. Jeder Sprint endet mit Tests und Anpassungen, so dass wir die App ständig verbessern, anstatt sie bis zum Ende zu optimieren.
Erst wenn alles so funktioniert, wie es soll - Leistung, Stabilität und Sicherheit -, stellen wir die App für psychische Gesundheit bereit und bringen sie in die Stores.
Bei Bedarf kümmern wir uns um Updates, Fehlerbehebungen und Sicherheitspatches und fügen neue Funktionen hinzu, wenn sich die Anforderungen der Benutzer ändern. Und warum? Eine App für psychische Gesundheit ist nicht statisch. Sie muss mit den Erwartungen der Nutzer Schritt halten.
Wir setzen unser Wissen in die Praxis um und helfen Ihnen, eine App zu entwickeln, die schnell ROI bringt.
Die Kosten für die Entwicklung einer App für psychische Gesundheit belaufen sich auf was Sie bauen und wie komplex sie ist. Eine einfache Wellness-App mit Tagebuchführung oder Stimmungsaufzeichnung liegt im unteren Bereich. Fügen Sie Videoanrufe, AI-gesteuerte Empfehlungen oder die Analyse von Patientendaten hinzu, und das Budget springt schnell in die Höhe. Wenn Sie eine AI-Diagnose oder ein Produkt der SaMD-Klasse für die psychische Gesundheit anstreben, müssen Sie mit erheblichen Investitionen rechnen.
Was meiner Erfahrung nach oft übersehen wird, sind die laufenden Kosten: Hosting, Wartung und Kundensupport. Sie sind nicht optional, aber sie müssen auch nicht aus dem Ruder laufen. Bei den Projekten, an denen ich mitgearbeitet habe, konnten wir die Budgets unter Kontrolle halten, indem wir uns frühzeitig für die richtige Technologie entschieden, wertsteigernde Funktionen in den Vordergrund stellten und dafür sorgten, dass das Team dem Umfang entsprach. Am klügsten ist es also, die Kosten mit jemandem zu planen, der das Projekt schon einmal durchlaufen hat. Auf diese Weise wissen Sie in jeder Phase, was auf Sie zukommt.
MedTech-Erfahrung seit 2007
100+ durchgeführte medizinische Projekte
Ein Team von 3,500+ Spezialisten, einschließlich derjenigen mit Erfahrung in AI, ML und Datenanalyse
Unverwüstlich und flexible Software-Architekturen die wachsende Nutzerzahlen bewältigen können
UX/UI-Design, das auf die Bedürfnisse von Patienten und medizinischem Fachpersonal zugeschnitten ist’ Bequemlichkeit
Übereinstimmung mit HIPAA, HITECH-Gesetz, GDPR, FDA, MDR, und andere Anforderungen
ISO 9001, ISO 27001, und ISO 13485-zertifiziert
93% von Kunden vertrauen Sie uns wieder und wieder
Die meisten Apps für psychische Gesundheit, an denen ich gearbeitet habe, benötigen mehrere Monate für die Entwicklung, aber der Zeitrahmen ist sehr individuell. Diese Spanne hängt davon ab, ob man ein leichtes MVP eines Stimmungstagebuchs oder etwas Komplexes mit Videoanrufen, AI-Agenten oder Therapien und Integrationen mit medizinischen Apps und Geräten entwickelt.
Wenn Ihre App Gesundheitsdaten von Patienten verarbeitet, ja, dann muss sie HIPAA-konform sein. Wenn es sich nur um einen Meditationsassistenten oder eine Stimmungs-Check-In-App ohne personenbezogene Daten handelt, fallen Sie vielleicht nicht unter den HIPAA, aber ich würde nicht riskieren, die Privatsphäre zu ignorieren. Bei meinen Projekten achten wir immer auf die Einhaltung der Vorschriften, denn es ist ein Albtraum, Verschlüsselung und Zugangskontrollen nachträglich einzubauen.
Das hängt von Ihren Zielen ab. Unsere Kunden fragen oft nach Dingen wie Videokonferenzen, Nachrichtenübermittlung, Symptomverfolgung und Integration von tragbaren Geräten. Weitere Funktionen, die sich lohnen, sind CBT-Übungen in der App, Peer-to-Peer-Unterstützung und vorausschauende Analysen von Krisensituationen.
Sie können eine App für psychische Gesundheit durch Abonnements, Freemium-Upgrades oder Partnerschaften monetarisieren. Abonnements funktionieren am besten, wenn die Nutzer einen kontinuierlichen Nutzen wie geführte Programme oder Therapiesitzungen erhalten. Mit Freemium können die Nutzer die Grundlagen ausprobieren und dann für erweiterte Funktionen bezahlen. Ich habe auch schon erlebt, dass Kliniken Apps als Teil der Patientenversorgung sponsern.
Der Markt für Apps für die psychische Gesundheit ist bereits eine Multi-Milliarden-Dollar-Branche und wächst schnell: 2024 wird er auf $7,23 Milliarden geschätzt und soll bis 2034 $32,05 Milliarden erreichen, mit einer CAGR von 18%. Im Moment ist die Nachfrage nach Apps zur Bewältigung von Depressionen und Ängsten am größten, aber ich sehe auch ein steigendes Interesse an Tools, die sich auf Stress und Burnout konzentrieren.

Portfoliomanager im Bereich Gesundheitswesen und Medizintechnik
Anastasiya Dziemieszkiewicz hat sich der technologischen Innovation im Gesundheitswesen verschrieben und ist die treibende Kraft hinter vielen der innovativen Projekte von Innowise - KI-Apps, digitale Gesundheits-Tools und vieles mehr. Sie arbeitet eng mit funktionsübergreifenden Teams und Unternehmen des Gesundheitswesens zusammen, um Lösungen zu entwickeln, die den Branchenvorschriften und den Zielen der Kunden entsprechen. Mit ihrem echten Interesse an der Verbesserung von Patientenergebnissen und Arbeitsabläufen im Gesundheitswesen beeindruckt Anastasia ihre Kunden immer wieder mit ihrem praktischen Ansatz und ihren frischen Ideen.










Ihre Nachricht wurde gesendet.
Wir werden Ihre Anfrage bearbeiten und uns so schnell wie möglich mit Ihnen in Verbindung setzen.

Mit der Anmeldung erklären Sie sich mit unseren Datenschutzrichtlinie