Your message has been sent.
We’ll process your request and contact you back as soon as possible.
The form has been successfully submitted.
Please find further information in your mailbox.


Across industries, legacy systems are showing their age, and companies are taking action. According to Statista, the surveyed companies said that the main reasons why they want to modernize their software are to improve security and efficiency, reduce costs, and integrate modern technologies.
To my mind, clinging on to legacy software in healthcare is riskier than in any other industry. Faulty software may not only slow down the hospital workflows, but, in the worst-case scenario, harm people’s health. Plus, rising patient and regulatory expectations are magnifying the need for modernization.
Yet, despite the clear benefits, modernization is often held back by tight budgets and the complexity of unwinding legacy code. This McKinsey report echoes what I see in the trenches: health systems want to transform processes and embrace new techs, but legacy systems are holding them back. To make modernization easier, I’ll walk you through the essentials in this article.
When I talk about legacy systems in healthcare, I’m usually referring to healthcare software that’s been around for 10–15 years. These solutions were built when things were different, so now the architecture and technologies they use may be outdated. Yes, they may still be functional, but soon enough, they won’t be able to support the pace of modern healthcare delivery.
However, taking a look at the software launch date is not enough to say it’s legacy. Working with many healthcare businesses, I’ve seen apps that have been around for 3–5 years, but already barely handle the load, can’t integrate with modern APIs, and use a dated tech stack. All because of the short-sightedness during the initial software design.
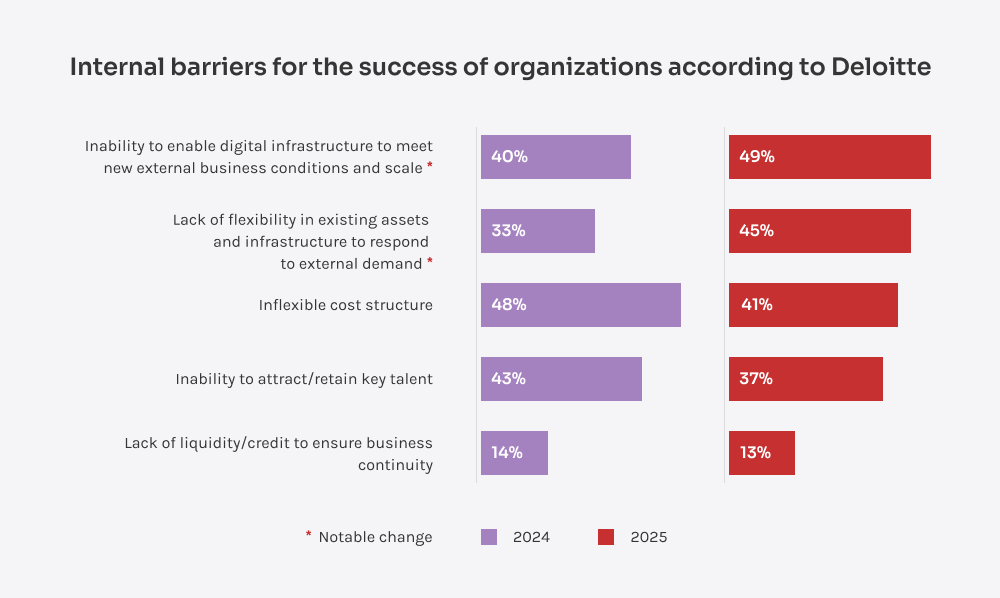
Sticking with legacy systems for too long creates a growing gap between what healthcare providers want to achieve and what their tech can actually support. For instance, Deloitte’s survey shows that 82% of companies missed cost-reduction targets, and half blamed that on outdated infrastructure. That statistic resonated with me because every time we at Innowise modernize healthcare software, we see significant cost reduction. And, on top of that, faster workflows, improved care delivery speed, and smooth interoperability.
Before jumping into healthcare software modernization, I always recommend starting with an audit, a software health check-up, so to speak. Just like you can’t plan treatment without a physical exam, you can’t plan modernization without understanding the state of the software.
While any type of healthcare software can become outdated, the ones listed below have typically been around the longest. That’s why, in my experience, they’re often the first to show signs of strain and likely need to be updated first.
EHRs are the backbone of clinical documentation, storing patient histories, diagnoses, prescriptions, and reimbursement data.
Why modernize: Legacy EHRs often rely on manual data entry only and lack proper interoperability and convenience. Modernized EHRs can be integrated with newer diagnostic tools, have built-in virtual assistants, support real-time data exchange, and overall are much easier to use.
Used in clinics, hospitals, and medical practices, these systems help structure and run daily work within a healthcare organization.
Why modernize: If you use a legacy practice management system, you risk stunting the efficiency of your practice. When modernized correctly, these apps can simplify and automate daily care and administrative operations. Plus, you get a chance to connect the practice management app to other IT systems and share information across your apps without delays and errors.
Widely adopted during the pandemic, these platforms offer remote consultations, messaging, and patient monitoring.
Why modernize: Early adopters of telemedicine systems may find their apps can’t handle user load (especially during peak video consultation activity) and often lack EHR integration. After modernization, telehealth apps usually have better video quality, seamless data sharing across systems. Additionally, data privacy and security are only reinforced during the updates.
LIS software manages lab workflows, test ordering, diagnostic results tracking, and sharing.
Why modernize: It’s hard for outdated LIS platforms to support the expected level of automation. With modernized LIS solutions, you increase throughput, reduce errors, and speed up result turnaround. Also, the amount of diagnostic equipment with its own software is ever-growing, so you need to make sure data is transferred to your legacy LIS correctly.
HIS platforms help handle administrative and clinical processes and data, from admissions to billing.
Why modernize: In my experience, legacy HIS apps are hard to scale and have less flexible functionality. When modernizing HIS software, I’d recommend implementing resource management features, financial tracking, and, naturally, integrations with other IT systems used.
RIS software is designed to manage workflows within a radiology practice or department: patient scheduling, results tracking, reporting, and more.
Why modernize: Older RIS solutions may seem isolated, as they rarely are properly integrated with EHR or HIS apps, leading to data silos, reporting delays, and lots of manual input. With modernized RIS, radiologists enjoy better data sharing and faster processes.
PACS apps help store and manage medical images, like ultrasounds, X-rays, MRIs, and CT scans.
Why modernize: I often hear that legacy PACS are harder to use for medical teams, so during modernization, you should focus on intuitive interfaces, faster image loading, and smoother image sharing between healthcare IT solutions.
These platforms vary from simple appointment booking apps to more sophisticated systems for chronic disease management.
Why modernize: If the app is complicated and slow, patients quickly get frustrated. Modernization can improve their satisfaction rates, thanks to convenient UX, mobile support, and smooth access to everything they need, like records, doctor schedules, and more.
With claims processing systems, organizations can handle billing, procedure coding, and communication with insurers.
Why modernize: Legacy platforms may take longer to process claims, so upgrades will help speed up claim handling, reduce billing errors, and improve revenue cycle visibility.
Deciding whether to maintain, modernize, or replace your healthcare software is a strategic decision. From what I know, sometimes, leaving things as they are makes sense, but often the hidden costs of inaction are larger than they first seem.
If your system is stable, performs reliably, and continues to meet user needs, there may not be an urgent call for modernizing healthcare software. Older systems can run smoothly, require minimal upkeep, and fit the workflows like a glove. Unless you want to add new functionality, in these cases, maintenance, periodic updates, and security checks are often the smartest choice.
But here’s the catch: even if software works properly, there can be pitfalls that haven’t manifested yet. In one of the projects I worked on, the legacy app was technically “fine,” but it required medical staff to do tons of manual work. The inefficiencies added up: not just in hours lost, but also in billing errors and the need for reworks. So even if your software “works,” it’s worth asking whether it’s enough for your healthcare business.
If your healthcare IT system shows any of the signs below, it’s a red flag, meaning you should seriously consider modernization.
| Performance issues preventing growth | You’re seeing frequent slowdowns, freezing, or even outages. Systems may grind to a halt during peak hours simply because they weren’t built to handle current loads. |
| Flawed security and compliance | When you’re patching vulnerabilities more often than you’d like or question compliance with HIPAA or GDPR, risks of breaches and fines are inevitable. Unless you take action. |
| Poor user experience | Patients and doctors complain about confusing interfaces or clunky processes. Clicking through tens of screens just to perform a single action is not okay. |
| Sky-high TCO with low ROI | If you're pouring money into healthcare software upkeep, but not getting proportional value back, it means your app requires substantial changes. |
| Insufficient functionality | You see growing dissatisfaction among users: the app can’t do what your medical team and patients need today, be it efficient reporting tools or convenient access from mobile devices. |
| Constant malfunctions | Errors, crashes, and unpredictable bugs shouldn’t become the norm for your healthcare business. Malfunctions are not just an inconvenience, they may affect care delivery and, worst of all, patient outcomes. |
| Hindered productivity | When performing tasks in the software takes longer than it should, you lose on the medical staff's productivity. |
| No vendor support for the software | In case you rely on the software that was abandoned or deprecated by a vendor, you’re sitting on a ticking bomb. Shifting to a new system is the way out that pays off in the long term. |
| Limited integration capabilities | If you can’t connect your legacy healthcare software with other systems, it requires a lot of manual operations and prevents you from adopting many innovative tools, like AI and wearable devices. |
| Tangled app workflows | Redundant tasks, broken processes, and manual data transfers — all these tiresome daily tasks can be forgotten after modernization. |
During healthcare modernization, there’s a range of strategies you can choose from, and each comes with its own benefits and trade-offs.
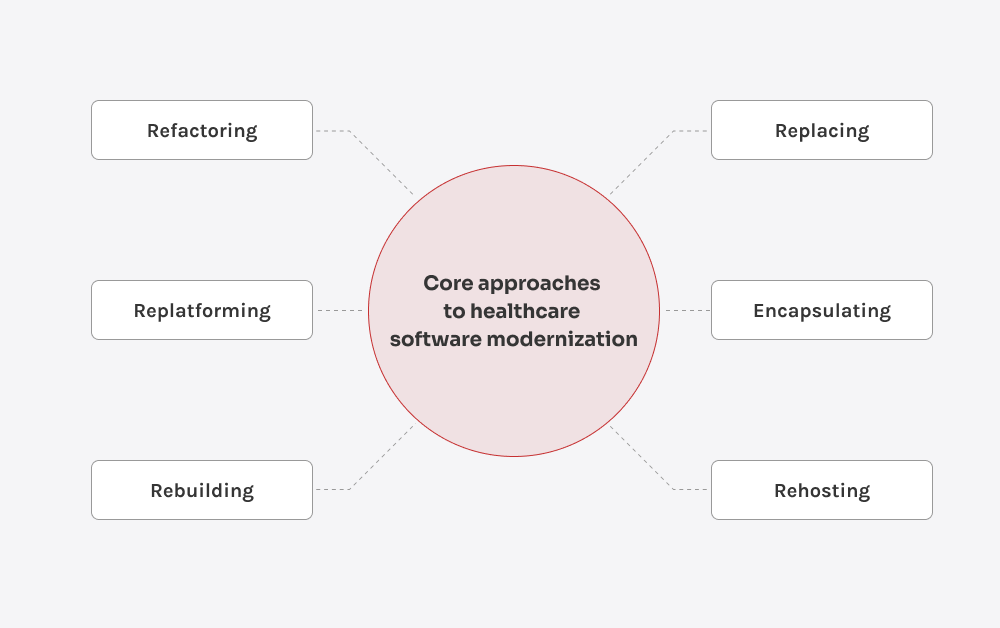
This approach basically means moving your existing healthcare software to new infrastructure, like switching from on-premise servers to the cloud, without touching the code.
Best for: Stable healthcare solutions that are still doing their jobs but can’t scale or meet performance needs.
Downsides: No functional or architectural improvements, existing code inefficiencies remain. You will still need to do manual patching in the cloud and, likely, need to partially refactor your app to fit the cloud environment.
Refactoring involves improving the internal structure of the code while keeping the healthcare solution’s functionality and logic the same.
Best for: Healthcare apps full of slapdash fixes and legacy patterns that work, but are becoming harder to maintain, update, or expand safely.
Downsides: No user-visible changes; the evident bugs are just the tip of the iceberg, so you may need to resort to a full app revamp. Plus, refactoring can sometimes be even more expensive than replacing the app.
With this approach, your healthcare software gets a newer tech stack, e.g., we shift from .NET Framework to .NET Core. Here, developers rewrite and adjust parts of the app to work better in the new conditions.
Best for: Organizations that want to modernize gradually, improve software performance, and get more flexibility without a full rebuild.
Downsides: Solution is still tied to legacy design; changes may disrupt integrations.
This is a full rewrite of the healthcare application using modern tools, frameworks, and architecture.
Best for: Healthcare software that is so outdated that a full rewrite will be more cost-effective than any short-term fixes.
Downsides: Temporary business disruptions, time-consuming process.
Sometimes, it’s better to go for a new off-the-shelf healthcare solution rather than trying to fix or rebuild the old one.
Best for: Non-business critical healthcare solutions with strong alternatives on the market.
Downsides: Vendor lock-in, lots of time and effort for user training, workflow changes, and insufficient functionality.
With this approach, you split the legacy codebase into pieces and add modern interfaces or features without touching the core of the healthcare IT system.
Best for: Organizations needing to modernize outward-facing functionality without risking system stability.
Downsides: Data-related issues, limited flexibility, and remaining technical debt.
When you modernize healthcare software, adding AI features along the way may help you bring the app to a whole new level. I often recommend that clients I work with update their outdated IT systems with these capabilities.
“Now that AI is truly thriving in the healthcare domain, the possibilities for modernizing medical apps with this advanced technology are endless. What I find especially beneficial is the ability of AI to automate routine tasks and free up time for more value-adding clinical activities.”

Portfolio Manager in Healthcare and Medical Technologies
Modernizing legacy systems in healthcare, like any complex IT initiative in this field, doesn’t come without its hurdles. Over the years, I’ve seen certain challenges appear time and again, so here are a few common roadblocks, along with ways to move past them.
Many of these issues can be avoided if you partner with a healthcare software modernization company like Innowise, as we’ve handled such risks successfully many times before.
While the challenges of modernization can often be mitigated with the right knowledge, continuing to run outdated healthcare systems poses far greater risks.
Outdated systems raise the chances of medical errors, misdiagnoses, and delayed care. What’s more, without modern data exchange protocols, even cross-department communication breaks down.
Legacy platforms often rely on dated security mechanisms, making them easier targets for cyberattacks and leading to staggering fines and legal troubles.
Frequent downtime, lagging response times, and outdated interfaces create bottlenecks that frustrate staff and slow down patient care.
Relying on legacy systems makes it harder to adopt advanced features, limiting your ability to streamline healthcare workflows and reduce operational costs in the long run.
Patients today expect digital access, fast communication, and personalized care. If you fail to meet the expectations, you may fall behind.
Over the last 18+ years in healthcare IT, Innowise’s team has helped modernize systems for hospitals, labs, and health tech startups around the globe. Here are a few projects that come to mind when I think about legacy software upgrades that led to tangible results.
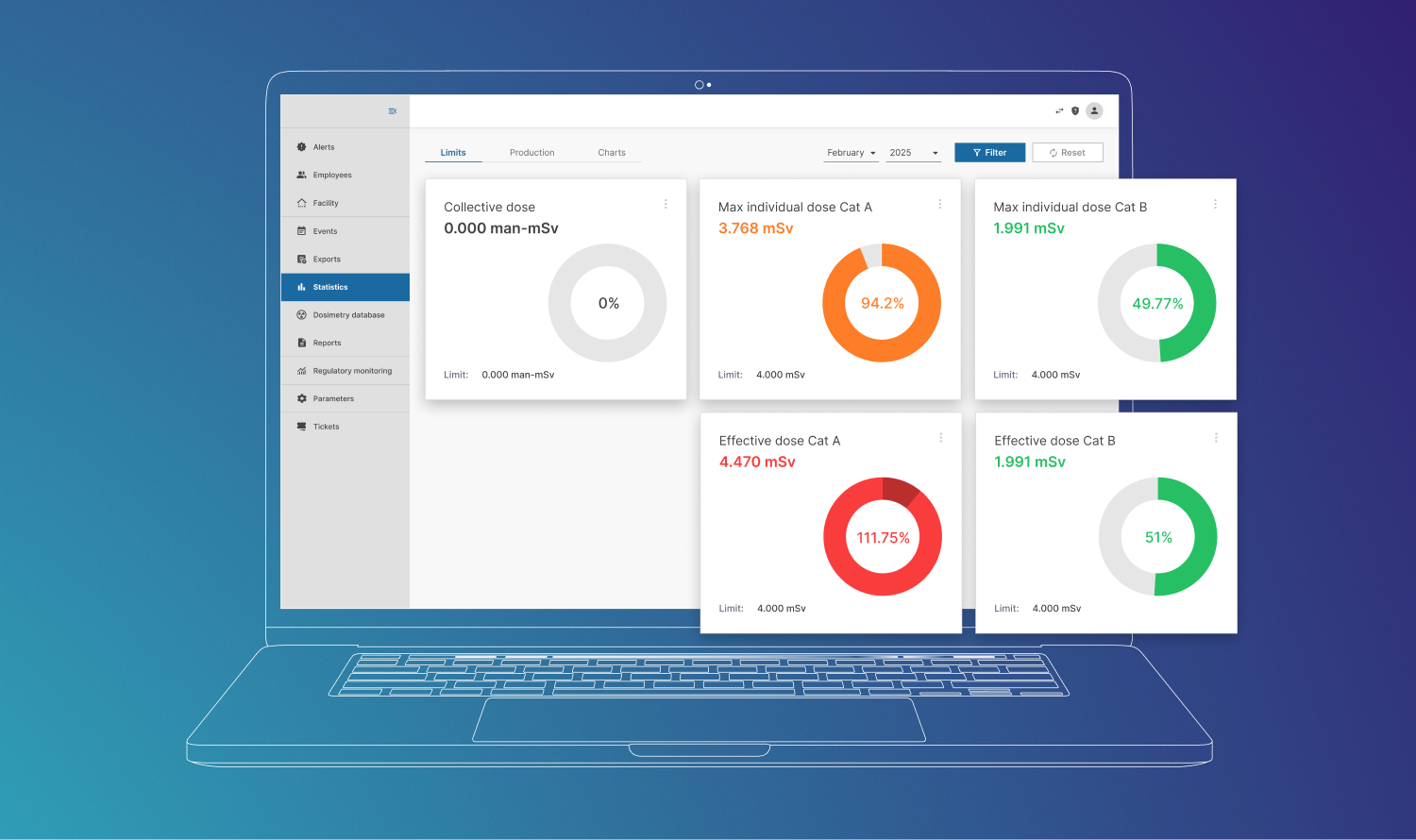
Innowise modernized a legacy radiation exposure monitoring app that was on the market for 10+ years. Thanks to the software infrastructure revamp, performance issues fixes, and tech stack modernization, the database performs 1.5–3x better, and the app responds 3.3x faster.
Working with a pharmacy chain, our team modernized the outdated inventory management system, replacing legacy code and implementing a microservices-based architecture. As a result, the system speed increased by 40% and overall throughput by 30%.
For a leading biotech company, we optimized the infrastructure of a lab management platform, automated DevOps, and enhanced CI/CD processes. It reduced compute costs by 70% and caused a x2 development speed increase.
With nearly two decades of experience in custom healthcare software development, Innowise can transform outdated medical systems into modern, scalable, and secure solutions.
Whether it’s upgrading an old EHR, refactoring a patient app, or rebuilding a practice management app, we tailor our approach to fit your needs and minimize disruptions. Innowise’s team is here to help you unlock the full potential of your healthcare apps thanks to legacy software modernization.

Senior Technical Delivery Manager in Healthcare and MedTech
Aleh has a strong grasp of what makes healthcare and MedTech software truly work. He leads with both technical clarity and sector knowledge, making sure every project delivers long-term value — not just code that runs, but systems that matter.








Your message has been sent.
We’ll process your request and contact you back as soon as possible.

By signing up you agree to our Privacy Policy, including the use of cookies and transfer of your personal information.